Disclaimer: On this page, we show pictures of patients which might be disturbing for some people. If you are sensitive that way, please don’t scroll down!
Felix suffers since birth form a severe constipation. Luckily for him, his parents lived close to the hospital, so that they found help to manage his condition with regular enemas. Nevertheless, hiss belly grew more and more, he himself lost substance continuously.
At our first visit, he was seven years old. We toke samples of his large bowel and created a colostomy, so that his intestines could recover. The samples were taken to prove our diagnosis, that a lack of neural cells in the large bowel stops it from moving normally. At our second visit, we were able to remove the bowel without nerve cells and close the colostomy.


At our last visit, Felix has gained substantially in weight, and no more problems in passing stool, his belly slowly gets back to normal, too.
Encouraged by the experience with this patient, at each visit some children of younger age are presented to us, who might have the same problem, and we were able to treat them, too, or at least start the treatment.
At the age of two years, Raminadatou drank by chance from the wrong bottle and burned here esophagus with leach. Following this incident, she was not able to eat or even drink any more. Our colleague on site created an access to her stomach through the abdominal wall, in order for her to be tube fed. With the equipment we brought along, we were able to dilate the esophagus, and the girl was able to eat porridge again.
We taught the local surgeon to perform this procedure, as it has to be repeated regularly over some months to keep the esophagus patent. He was continuing this treatment up to the last visit, and a special donation allowed the family to pursue this treatment, which otherwise would have been beyond their financial possibilities.



In the meantime, Raminadatou has had a serious pneumonia and pleural empyema, but recovered well. She needs treatment less then once a month and is well nourished. The Gastrostomy has been closed, as she is feeding completely by mouth.
Taibatou was born with this neck tumor, and she was presented to us at the age of six weeks.
During the operation, the tumor was completely excised without injury to the surrounding structures.
The histological exam showed no malignancy in the tumor.


Abdou is born with a open back or spina bifida, where the neural tissue was only covered by a thin layer of skin. As the defect is very low on the back, the nerves to the lower limbs and the pelvis are probably not affected.
At the operation, the back was completely closed.
Abdou needs to be followed up closely, as after closure, there might develop a hydrocephalus, which also will need surgical attention.
Rachidou already has a marked hydrocephalus.
For a normal development of the child it is mandatory to drain the cerebrospinal fluid, usually into the abdomen. This helps that the head doesn‘t get to heavy, and the brain doesn‘t suffer from pressure.
On operation, a valve is implanted, the function of which needs regular control. On long term, this only makes sense if we are able to establish regular pediatric surgical care. As those valves are quite expensive, we depend on donations for these operations, too.
We are sorry that Rachidou missed her scheduled operation!


Salifou has suffered a burn to her right shoulder as a toddler and is not able to move it any more.
During an elaborate operation, the contracture was released, and a skin flap brought into the axilla to make the shoulder mobile again.
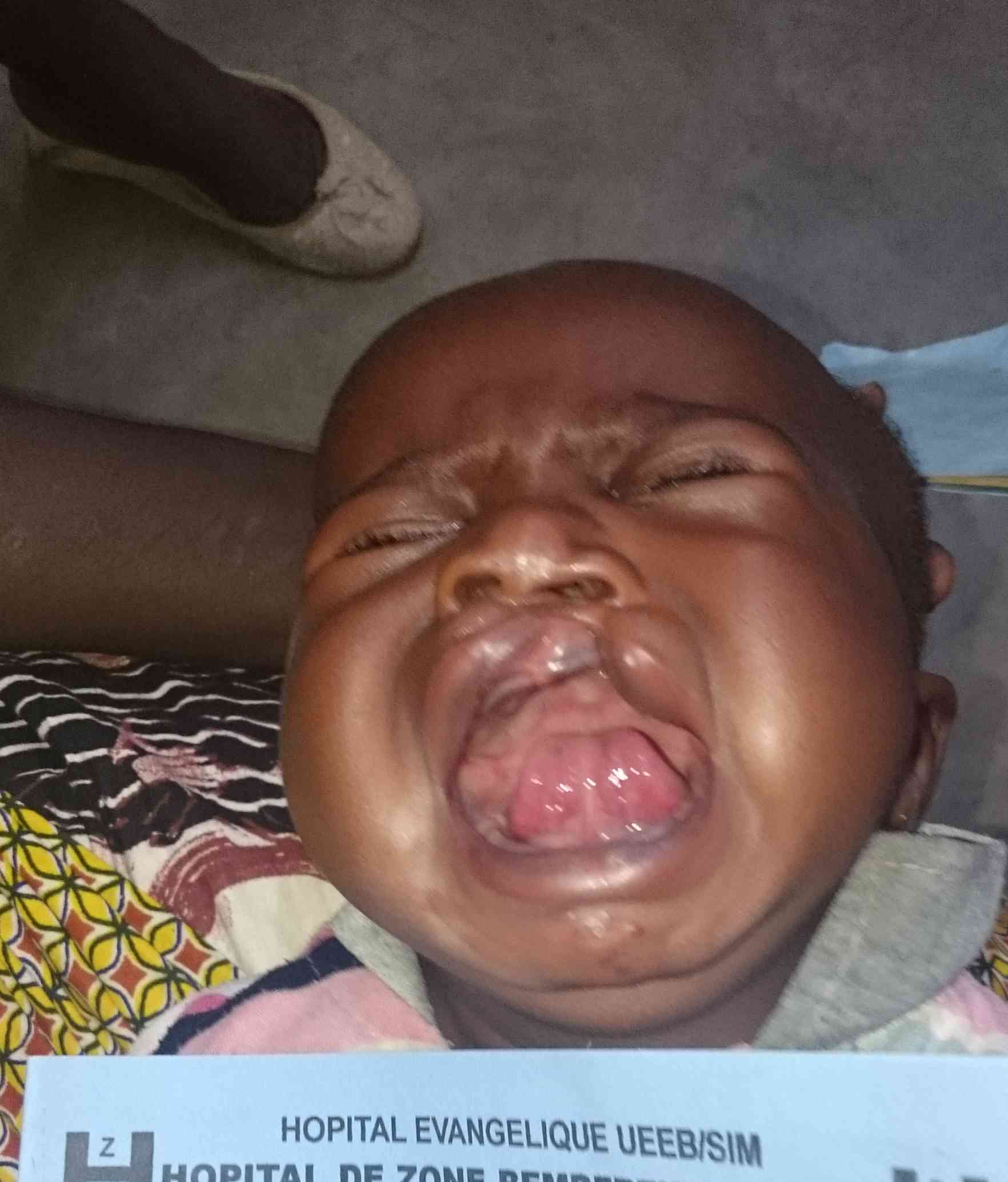
Bassina suffers from Noma, a disease with massive tissue destruction involving the face mostly. Malnourished children who are not vaccinated against measles are mainly at risk for this disease. Luckily for her, she was treated in time and survived the acute phase of the disease. 90% of the patients don’t.
For the time beeing, she is in nutritional rehabilitation, and we hope to restore her face during one of the future missions.


Martine had a very serious inflammation in her abdomen, and needed several abdominal operations including a temporary ileostomy. After healing, she developed a huge incisional hernia. We were able to close this for a more normal looking abdomen.
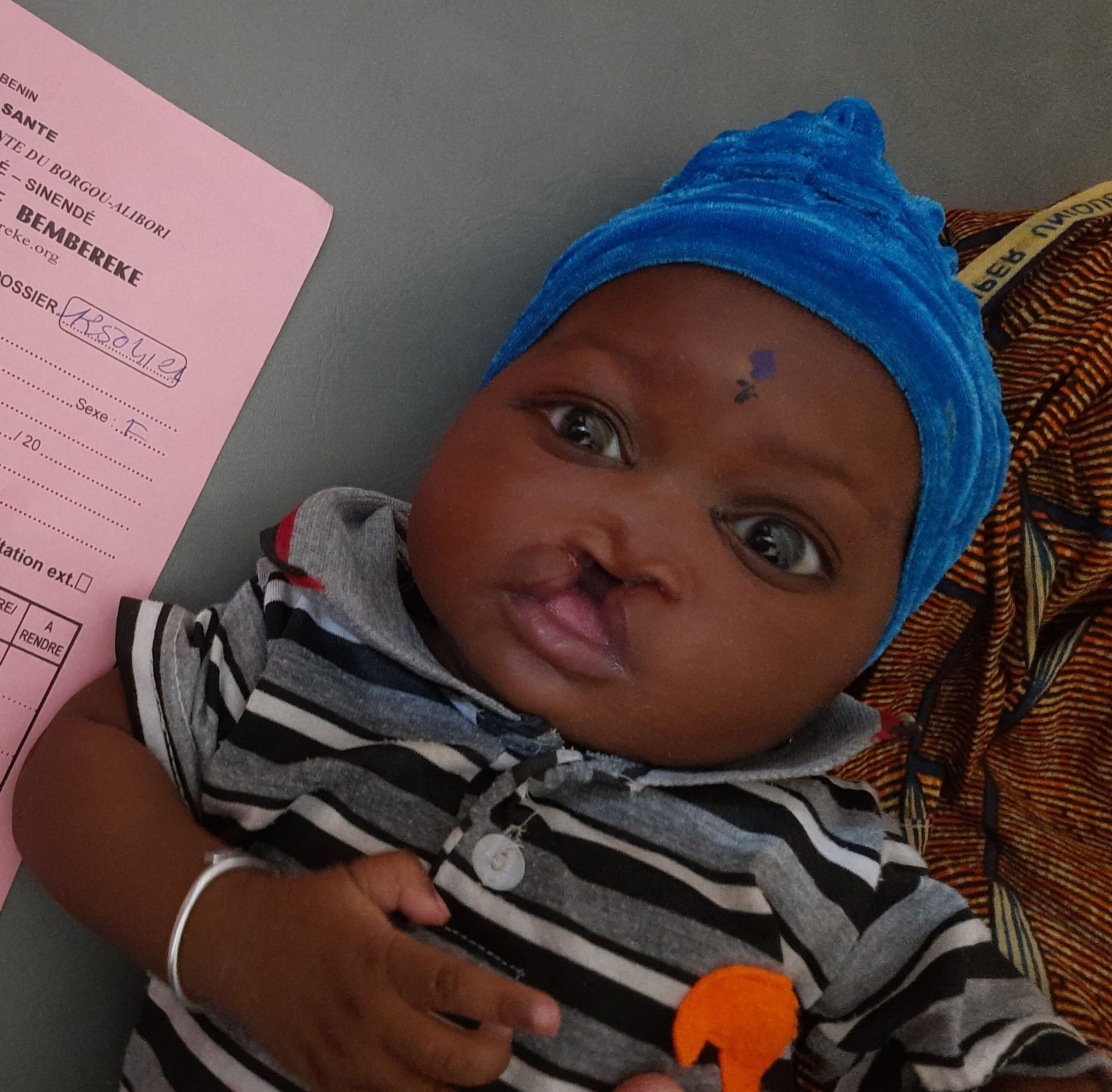
Cleft Lip and Palate
Since the beginning of our missions in Bembèrèkè, we have also operated on children with clefts every time and used this opportunity to teach our colleague Dr. Jonathan Troukou these surgical methods.
These interventions are supported by Smile Train.